Dental Disease In Dogs: A Dentistry Expert's Guide

Written by Dr Shula Berg & Dr Jose Carlos Almansa Ruiz
Medically reviewed by Dr Paul Higgs
Table of Contents
- Introduction
- Interesting Facts
- What does a healthy mouth look like?
- Symptoms of dental disease
- Types of dental disease
- Risk factors
- Diagnosis
- Treatment
- Dental procedures
- Prevention
More than 70% of dogs over 3 years old have dental disease, though this can vary from mild to severe. Almost all pets will, at some point, benefit from having a dental procedure to clean and assess the teeth, and remove any that are diseased or damaged. Often, this needs periodically repeating to maintain a healthy mouth. However, a dog having their teeth cleaned every two years is like us visiting the dentist once every 14 years!
Oral health is not only important for making sure your dog's mouth is comfortable, but can protect the rest of the body too. Bacteria harboured in oral infections can enter the blood stream and travel to other organs, causing problems much more serious than bad breath. This is important since dental disease is the most common group of conditions diagnosed in dogs in the UK[2].
Under the umbrella of dental disease, we encounter several conditions such as gum disease, fractured teeth and malocclusions, to name but a few. We've turned to Dr Jose Carlos Almansa Ruiz a recognised expert in the field of veterinary dentistry, to tell us a bit more about the oral cavity of dogs, the most common problems, and how to prevent them.
Interesting facts about oral cavity of dogs
- An adult dog has 42 teeth – made up of 12 incisors, 4 canines, 16 premolars and 10 molars.
- Only approximately 5% of dogs suffer from tooth decay, partly because a dog’s saliva is much more alkaline than a humans – the typical pH of canine saliva is 7.5-8, compared to 6.5-7 in people.
- Tooth enamel is the hardest structure in the body; in canine teeth, thickness ranges from 0.1-0.6mm thick, which is a lot thinner than the 2-4mm thickness found in humans.
- The roots of the canine teeth (sitting within the jaw) can be as long as 4cm!
- In small and toy breeds of dog, the roots of the first molar teeth in the lower jaw are almost as long as the height of the jawbone.
- On the roof of the mouth, the soft tissue covering the hard palate makes a pattern which is unique for each dog, almost like our fingerprints.
- Some dogs have hair on their tongues, and this is completely normal!
- Unlike some other animals, dogs are not able to move their lower jaw from side to side due to the anatomy of the joints holding the lower jaw to the rest of the skull.
What does a healthy mouth look like?
When looking inside your dog´s mouth, the following findings suggest the mouth is healthy:
- When teeth first erupt into the oral cavity, the colour of the enamel is white. The most common cause for discolouration is build-up of plaque and tartar, though exposure to certain drugs as a puppy, or rarely, trauma to the tooth (concussion), can affect the colour.
- Upper and lower teeth should meet each other without causing damage to the teeth or soft tissues. Normally, the upper incisors slightly overlap the lower incisors, known as the scissor bite.
- The crowns (visible parts) of the teeth should have smooth edges with no parts missing.
- The gums should be uniform, pink in colour, and not showing signs of bleeding.
- All the soft tissue surfaces (such as inside the cheeks) in your dog´s mouth should have a nice pink appearance, with no growths or ulcers visible. Some breeds, such as the Chow Chow or Shar Pei, can have pigmentation of these tissues, giving them a much darker appearance.
What are the symptoms of dental disease in dogs?
Dogs can show a variety of symptoms with dental disease. However, some dogs will show no symptoms at all. Dental disease progresses gradually, and some dogs will continue to eat even with extremely painful mouths. This is one of many reasons that regular dental checks are essential to be sure your dog’s mouth is healthy and free from pain.
Some common symptoms that could suggest dental disease include:
- Eating less than normal or eating more slowly than normal
- Dropping food out of their mouth or around the bowl
- Bad breath
- Redness of the gums
- Drooling more than normal
- Inability or unwillingness to open the mouth
- Bleeding seen in the mouth, or blood present on toys or bedding
- Pawing at the face
- Sudden swelling of the face, especially around the cheek
- Non-healing wounds on the skin surrounding the muzzle
What are the different types of dental diseases that dogs can get?
The most commonly diagnosed disease in dogs in the UK is periodontal disease, commonly known as gum disease. Other types of dental disease seen in dogs include;
- Damaged teeth
- Malocclusions
- Canine Chronic Ulcerative Stomatitis (CCUS)
- Tumours affecting the teeth and gums
- Tooth resorption
- Fractures of the jaw (can be related to infection around the teeth)
- Tooth root abscesses
- Retained deciduous (baby) teeth
- Developmental problems (such as unerupted teeth or problems with occlusion)
Periodontal Disease
Build-up of bacteria in the mouth leads to inflamed gums (Gingivitis) and, if left untreated, damage to the supporting tissues of the teeth. Periodontal disease is likely to affect all dogs during their lifetime, but is most commonly seen in the UK in Schnauzers and Greyhounds.
Dental disease is a slow process which develops over many months. The stages of dental disease are:
Plaque |
Gingivitis |
Periodontitis |
 |
 |
 |
|
Plaque is the layer of bacteria found across the surface of the tooth, and is what makes our teeth feel fuzzy if we don't brush. It develops within a few hours of cleaning and, if left, becomes a thick, visible layer known as tartar. |
Plaque build-up causes inflammation of the gums, seen as redness starting from the tooth margin and radiating outwards. Eventually, Gingivitis will cause the gum edge to lift off the tooth, creating a pocket in which bacteria can multiply. |
Periodontitis means inflammation and infection of the ligaments and bone supporting the teeth. This causes the tooth roots to become exposed and eventually, teeth become loose. Periodontitis will cause chronic pain if left untreated. |
It is important to understand that Gingivitis can be reversed to a healthy gum status with the right care. Once Periodontitis has developed, this becomes a chronic condition, and we see alternating periods of active tissue destruction with periods of inactivity. Periodontitis is irreversible and can be controlled but not cured.
Rarely, if dental disease is severe and untreated, bacteria from the mouth can enter the blood stream. They can then travel around the body, causing illness elsewhere such as the heart, liver or kidneys. Although this is uncommon, it can make pets seriously unwell and even be life-threatening.
Damaged Teeth
Injury to the teeth can occur from inappropriate toys or chews, blunt trauma (such as being hit by a frisbee while attempting to catch it), or due to other types of accident (such as being hit by a car or fighting with another animal). Damage to the enamel (hard coating of the teeth) can lead to the sensitive pulp cavity in the centre of the tooth being exposed.
Exposure of the pulp cavity, either by a sudden traumatic fracture or rapid wearing of the tooth, can allow the bacteria in the oral cavity to infect and overwhelm the natural defence mechanism of the pulp. This causes the pulp tissue to die off; a painful process that may continue for months after the event. Initially, infection of the pulp is a sharp pain, but this often becomes a more dull and prolonged type of pain. In people, this requires a root canal treatment to remove the infected pulp and fill the remaining canal.
Dogs that commonly carry tennis balls in their mouths will show signs of chronic wear of the enamel. If this happens slowly, the tooth can produce a specific type of dentine (the layer below the enamel) called tertiary dentine. This protects the pulp cavity from being exposed and the tooth will remain healthy. If the wearing process is fast, the tooth will not have time to protect itself, resulting in the process described above.
Less commonly, if a tooth is subjected to blunt trauma, the tooth may not fracture but the soft tissues within the root canal can bleed and become inflamed. These tissues are enclosed in a rigid case that can’t flex with swelling, meaning pressure builds up inside the tooth and blocks blood flow. As a result, the tooth eventually ends up dying; commonly causing discolouration due to blood invading the tubules of the dentine. Initially the tooth will have a pink colour before this changes to a grey/black colour later on.
All teeth that have pulp exposure should be treated promptly, as infection will be painful and cause irreversible damage. Fractured teeth can be treated by extraction or root canal therapy, however, the latter is usually only performed by dental specialists or vets with advanced dentistry training. Although most teeth can be extracted without problems, it is worth considering root canal treatment for major teeth such as the canines and carnassials, especially in young, healthy dogs.
Malocclusions
Malocclusion means that the teeth are not properly aligned. The length of the upper and lower jaws, and the position that teeth erupt, are controlled genetically. Breeding of dogs for certain “looks” have changed the relationship, and length of the jaws, leading to malocclusions. This is especially common in dogs with short faces (brachycephalics) such as Pugs, Bulldogs and Shih Tzus.
When your dog closes their mouth, it is important to look whether there is any contact between the upper and lower teeth, or between any of the teeth and the soft tissues of the mouth. If there is contact between the teeth, the bigger teeth may displace the smaller ones, or affect the wear of the outer or deeper layers of these teeth. When the contact occurs between teeth and soft tissues, this will result in the formation of painful ulcers. In more severe cases, teeth that damage the tissues on the roof of the mouth can result in the formation of a connection between the oral and nasal cavity (an oronasal fistula).
Much like in humans with orthodontic treatment, correction of malocclusion can be complex and slow. Treatment of malocclusion in dogs can start when the baby teeth are still present, at 2-4 months of age. If the problem remains once the permanent teeth have erupted, movement of the affected teeth can still be possible in patients up to 12 months of age. Alternatively, other treatment options are available for patients older than a year of age, or in cases in which the movement of these teeth is not possible. Generally, treatment of malocclusion is undertaken by a dental specialist or a vet with advanced dentistry training.
Canine Chronic Ulcerative Stomatitis (CCUS)
This disease was known in the past as Canine Chronic Paradental Stomatitis. It most commonly affects Maltese and Scottish Terrier breeds, but very little is known about why it occurs. CCUS causes ulcers on the inside of the lips, edge of the tongue, and roof of the mouth. These ulcers can be quite large and deep, and in extreme cases, can affect the jaw bone. It is believed that the ulceration could be triggered by the dental plaque present on the surface of the teeth, although some ulcers may remain in place in areas where no teeth are present. Good oral hygiene is essential, together with pain killers, to control this disease. Other medications are available that, used together with oral hygiene, can help revert the inflammatory status.
Some affected dogs that do not tolerate tooth brushing may require the extraction of some or all the teeth in order to remove the areas that dental plaque occurs in the mouth. Despite this, some dogs will still need medical treatment as well to control this disease.
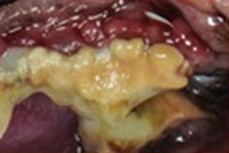
Oral Tumours
Tumours of the oral cavity represent around 5-7% of all tumours diagnosed in dogs. Many different types of tumour can affect the tissues of the mouth, and these appear in many different ways; from an extraction site that does not heal as expected, to a typical mass arising from the gum tissue. Treatment options will depend on the type of tumour diagnosed but may include surgical excision, chemotherapy or radiotherapy, or a combination of the three.
Tooth Resorption
Loss of teeth is a normal process for deciduous (baby) teeth, and occurs due to destruction of their roots, allowing the teeth to fall out. This process can happen to permanent (adult) teeth, but is never normal. There are certain situations where the dog's own body will attack their teeth, such as when there is infection in or around a tooth or, less commonly, cancer is present near the teeth. In some dogs, destruction of teeth may take place without a known reason, known as idiopathic resorption. Tooth resorption, idiopathic and due to inflammatory causes, affects around 50% of dogs.
Resorption of the tooth may take place below the gum level (the tooth root) or above the gum level (the crown). If above the gum level, the destruction of the tooth structure will eventually result in the exposure of the dental nerve, causing pain until the tooth is either extracted, or eventually lost due to the progression of the destruction process. Patients may show signs of oral pain, such as pawing at the face, eating slower or refusing to eat dry food. Resorption below the gum level can also be painful, and can be seen on dental x-rays.
What are the risk factors for dental disease?
There are several risk factors that increase the likelihood and severity of dental disease. Some of these we can control, while others are simply good to be aware of:
Risk factors you can control:
- Lack of regular dental care (such as tooth brushing)
- Diet consisting of mainly soft food
- Damage to teeth from chewing hard objects such as stones and antlers
Risk factors you can’t control:
- Breed; smaller dogs have an increased risk of dental disease, especially Toy Poodles, King Charles Spaniels, Greyhounds and Cavalier King Charles Spaniels[2]
- Age[2]
How is dental disease in dogs diagnosed?
Diagnosing dental disease in dogs involves specific steps and techniques.
Clinical exam
The initial step in diagnosing dental disease is a clinical examination by a veterinarian or veterinary nurse. They can identify signs of dental disease and its severity during this exam, determining whether the dental disease is mild, moderate or severe.
Complete mouth assessment
For a thorough diagnosis, a complete assessment of the dog's mouth is necessary. This is typically done under general anesthesia as it allows for a detailed examination, even in well-behaved pets. Dogs have 42 teeth, each of which will be cleaned and examined and the findings recorded.
X-ray
Only the crown of the tooth sits above the gum-line; the tooth roots sit within the jaw and can be as large as or longer than the crown. To fully assess both the roots and the jaw-bone around them, x-rays are required. It may be recommended to take x-rays of your dog’s whole mouth, or just any diseased teeth.
What treatments are available for dental disease?
Effective treatment of dental disease in dogs is crucial for alleviating discomfort and preventing further health complications.
Home care for mild cases
Dogs with mild dental disease, characterized by little or no tartar, can often be managed with diligent home care, including regular teeth brushing to slow down the progression of the disease.
Dental procedures for moderate cases
Dogs with moderate tartar buildup or mild Gingivitis usually require a dental procedure to resolve these issues and prevent them from worsening. This procedure is typically recommended within three months of the initial examination. Following the procedure, ongoing home care is essential to delay the recurrence of dental disease.
Immediate procedures for severe cases
In cases of Periodontitis, which indicates severe dental disease, an immediate dental procedure is advised. Periodontitis is a painful condition, and if left untreated, there's a risk of infection spreading from the mouth to other parts of the body.
A fixed price for dental treatment is one of the benefits included when you join The Healthy Pet Club.
FIND OUT MORE ABOUT THE HEALTHY PET CLUB
What if a dental procedure is recommended?
If the vet or nurse advises your dog would benefit from a dental procedure, there is a good chance that ignoring this will cause worsening of the dental disease and potential discomfort for your dog. This means that when the procedure is eventually performed it will be more complex, probably taking longer and costing more. There is a greater chance that more teeth will require extraction. By acting early, we have a much better chance of restoring oral health and preserving teeth.
Dental procedures in dogs are always performed under anesthetic, as it is simply not possible to do a thorough clean with pets awake. Although no anesthetic is completely risk-free, we use personalised drug protocols for each individual patient, along with experienced staff and high-spec monitoring equipment to make the procedure as safe as possible. If you have specific concerns about your pet having a dental procedure, please speak to a member of the team. We are happy to answer any questions you may have.
How to prevent dental disease in dogs
Much like in people, it is impossible to completely prevent dental disease, and all animals will naturally develop some tartar with age. Some breeds are much more likely to suffer with bad mouths, especially toy breeds such Chihuahuas and miniature poodles, sight-hounds and terriers. There are several things we can do to help prevent development of Gingivitis and Periodontal Disease:
Regular oral health check-ups at home
It is essential to regularly open and look at your dog’s mouth at home. Check for bad smells (especially if this is worse than normal), broken teeth, and redness of the gums. Even if you aren’t confident looking at the teeth, doing this regularly will get your dog used to having their mouth examined. This means the vet or nurse is more likely to be able to have a good look in the clinic, without your dog being worried about what is happening.
Regular oral health check-ups with your vet
Ideally, we want to identify dental disease in the earliest stages so that we have the best chance of intervening, keeping the mouth healthy and preserving the teeth. Spotting the first signs of dental disease is best done by a trained professional, during regular check-ups with a vet or nurse. These should happen every 6 months, or sooner if you have concerns.
Oral health care at home
There are several things you can do at home to help keep your dog’s mouth healthy, and dramatically slow down the progression of dental disease:
- Brushing: As with ourselves, regular brushing is the best way to keep teeth healthy. Most pets can be taught to accept tooth brushing, but younger pets tend to learn faster than older animals.
- Rinses and gels: Various oral rinses and gels are available, most containing Chlorhexidine to reduce bacterial load and plaque. Many are effective; look for products with the VOHC (Veterinary Oral Health Council) seal or see their website for a list.
- Diet: Dogs fed dry biscuit diets have less tartar than those fed only on wet food. This is because the action of crunching biscuits causes abrasion against the teeth, helping reduce plaque build-up.
- Chews and toys: Dental chews and toys create abrasive action on the teeth to reduce plaque and tartar build-up. Chews should be factored into daily feeding to prevent weight gain.
Summary
Dental disease is one of the most common health problems seen in dogs. Left untreated, it will progress causing pain, discomfort and potentially serious consequences. A pro-active approach is essential to keep your dog's mouth healthy, including at-home care and regular dental checks with a vet or nurse.
References
[1]Enlund, K.B., Brunius, C., Hanson, J., Hagman, R., Höglund, O.V., Gustås, P., and Pettersson, A. (2020) Dog Owners' Perspectives on Canine Dental Health—A Questionnaire Study in Sweden. Sec. Veterinary Dentistry and Oromaxillofacial Surgery, Front. Vet. Sci., Volume 7. https://doi.org/10.3389/fvets.2020.00298
[2]O’Neill et al. (2021) “Epidemiology of periodontal disease in dogs in the UK primary-care veterinary setting”, Journal of Small Animal Practice. Volume 62, Issue 12 Pages 1051-1061. 10.1111/jsap.13405
[3]O’Neill, D.G., James, H., Brodbelt, D.C. et al. Prevalence of commonly diagnosed disorders in UK dogs under primary veterinary care: results and applications. BMC Vet Res 17, 69 (2021). https://doi.org/10.1186/s12917-021-02775-3
Disclaimer
Please note that the content made available on this webpage is for general information purposes only. Whilst we try to ensure that at the time of writing all material is up to date and reflects industry standards, we make no representation, warranties or guarantees that the information made available is up to date, accurate or complete. Any reliance placed by yourselves is done so at your own risk.
Related Articles & Services

